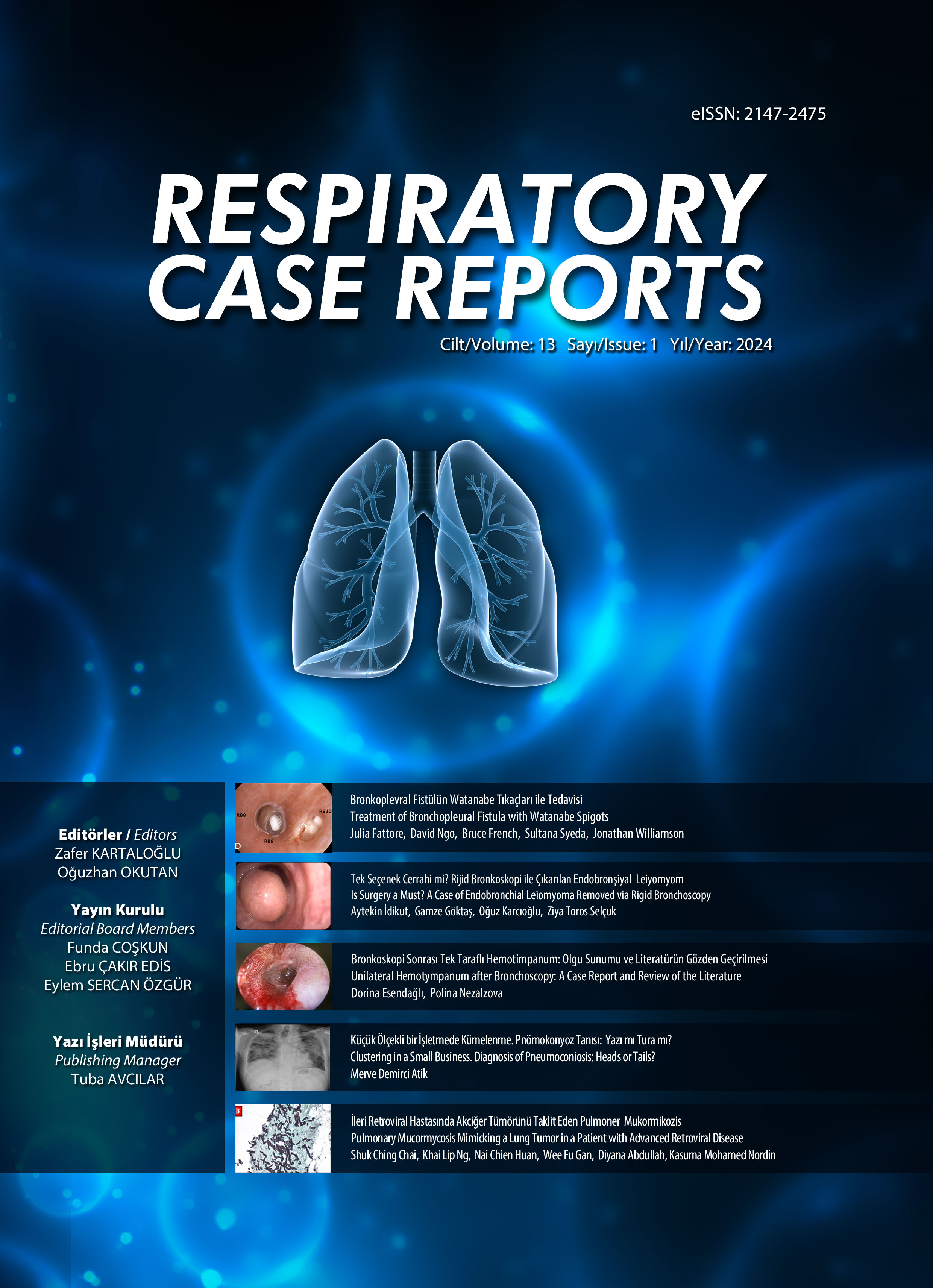
Masif Pulmoner Hemorajinin Nadir Bir Nedeni: İnvaziv Aktinomikoz
Bilge Yılmaz Kara1, Mehmet Fatih İnecikli2, Melek Memoğlu1, Recep Bedir4, Uğur Kostakoğlu3, Songül Özyurt1, Gökçen Sevilgen5, Şule Batçık6, Ünal Şahin11Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Göğüs Hastalıkları Ana Bilim Dalı, Rize2Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Radyoloji Ana Bilim Dalı, Rize
3Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Klinik Mikrobiyoloji ve Enfeksiyon Hastalıkları Ana Bilim Dalı, Rize
4Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Patoloji Ana Bilim Dalı, Rize
5Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Göğüs Cerrahisi Ana Bilim Dalı, Rize
6Recep Tayyip Erdoğan Üniversitesi Tıp Fakültesi, Anestezi ve Reanimasyon Ana Bilim Dalı, Rize
Pulmoner aktinomikoz geç tanı konulduğunda ölümle sonuçlanabilecek bir durumdur. Daha çok immün yetmezliği olan bireylerde beklenebileceği gibi immünkompetan kişilerde de görülebileceği unutulmamalıdır. Bu yazıda invazif pulmoner aktinomikoza bağlı masif pulmoner hemoraji gelişen nadir bir olgu sunulmuştur. Elli iki yaşında bilinen immünsupresif durumu olmayan erkek hasta ağızdan balgamla karışık kan gelmesi nedeni ile yatırıldı. Bronkoskopi planlanan hastanın genel durumunda ani kötüleşme nedeni ile çekilen toraks bilgisayarlı tomografisinde sol akciğerde başvuruda olmayan total atelektazi saptandı. Yoğun bakım ünitesinde yapılan acil bronkoskopide sol ana broşta masif hemoraji her iki ana bronş mukozasında yaygın nekrotik görünüm izlendi. Alınan mukozal biyopsinin patolojik incelemesinde aktinomikozla uyumlu gram pozitif filamentöz bakteri agregatları izlendi. Bronşiyal arter kateterizasyonunda ekstravazasyon saptanan artere embolizasyon işlemi uygulandı. Ancak takiplerinde gelişen bilateral nekrotizan pnömoni nedeni ile hastanın yoğun bakım takibine devam edildi. Hasta IV penisilin G ve anti fungal tedaviye rağmen 40 günlük takip sonrasında kaybedildi. Masif pulmoner hemoraji olgularında sıklıkla kanama yapan hastalıklar ve tümoral lezyonların yokluğunda ayırıcı tanıda aktinomikoz gibi anjioinvazif enfeksiyonlar düşünülmelidir.
Anahtar Kelimeler: aktinomikoz, masif pulmoner hemoraji, nekrotizan pnömoniA Rare Cause of Massive Pulmonary Hemorrhage: Invasive Actinomycosis
Bilge Yılmaz Kara1, Mehmet Fatih İnecikli2, Melek Memoğlu1, Recep Bedir4, Uğur Kostakoğlu3, Songül Özyurt1, Gökçen Sevilgen5, Şule Batçık6, Ünal Şahin11Recep Tayyip Erdogan University Faculty of Medicine, Department of Pulmonology, Rize, Turkey2Recep Tayyip Erdogan University Faculty of Medicine, Department of Radiology, Rize, Turkey
3Recep Tayyip Erdogan University Faculty of Medicine, Department of Infectious Diseases, Rize, Turkey
4Recep Tayyip Erdogan University Faculty of Medicine, Department of Pathology, Rize, Turkey
5Recep Tayyip Erdogan University Faculty of Medicine, Department of Thoracic Surgery, Rize,Turkey
6Recep Tayyip Erdogan University Faculty of Medicine, Department of Anethesiology and Reanimation, Rize,Turkey
Pulmonary actinomycosis is a severe clinical condition that may cause death if unrecognized. It may occur in patients who were previously healthy or may develop in patients with chronic immunosuppressant conditions. Presently described is a rare case of massive pulmonary hemorrhage with a related angioinvasive Actinomyces infection. A 52-year-old formerly immunocompetent man was admitted to the hospital due to blood-streaked sputum. A computed tomography image of the thorax taken after the patients clinical status suddenly worsened revealed total collapse of the left lung. No tumoral lesion was observed, but extensive necrosis of the mucosa of both main bronchi with massive hemorrhaging in the left main bronchus was seen in an urgent bronchoscopy performed in the intensive care unit. A histopathological examination of the mucosal punch biopsy demonstrated aggregates of filamentous Gram-positive organisms indicating Actinomyces infection. Selective embolization of a branch of the feeding artery was successful to control the hemorrhage, but necrotizing pneumonia emerged and the patient could not be discharged from the intensive care unit. He was later lost despite 40 days of treatment with intravenous penicillin-G antifungal therapy. Pulmonary angioinvasive infections like actinomycosis must be kept in mind in the absence of bronchial carcinoma or other frequently encountered diseases in cases of massive pulmonary hemorrhage.
Keywords: actinomycosis, massive pulmonary hemorrhage, necrotising pneumoniaOlgunun Görüntü Kesitleri
Sorumlu Yazar: Bilge Yılmaz Kara, Türkiye
Makale Dili: İngilizce