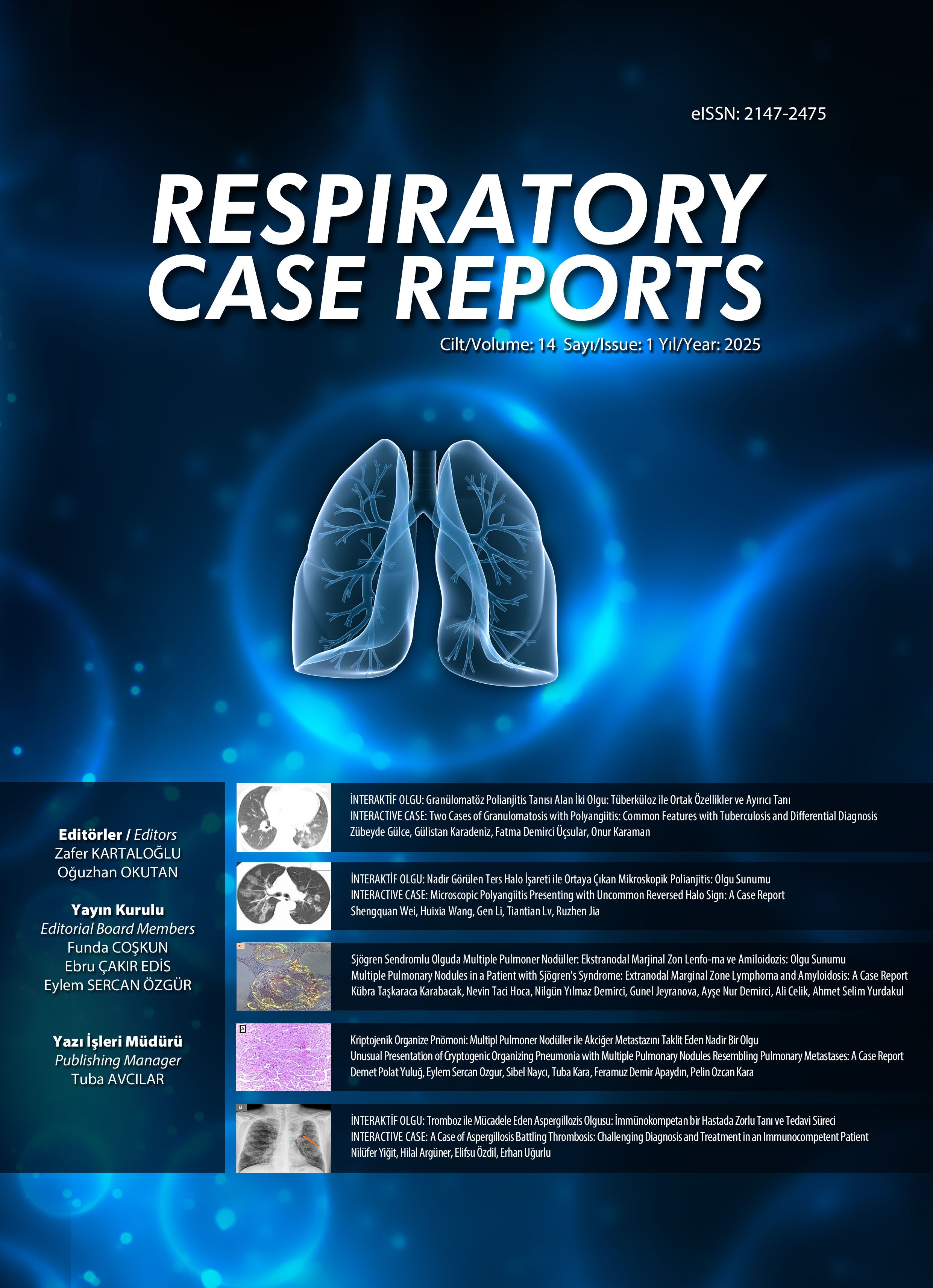
e-ISSN 2147-2475

Cilt: 2 Sayı: 1 - Şubat 2013
| KAPAK | |
| 1. | Kapak Cover Sayfa I |
| KÜNYE | |
| 2. | Künye Editorial Board Sayfa II |
| OLGU SUNUMU | |
| 3. | Mesalamine Bağlı Akciğer Toksisitesi Lung Toxicity Due To Mesalamine Ali İhsan Yıldız, Sibel Özkurt, Göksel Kıter, Zahide Alaçam, Belgin Erkan Aydoğandoi: 10.5505/respircase.2013.43531 Sayfalar 1 - 5 Mesalamin, inflamatuvar barsak hastalıkları tedavisinde kullanılan bir ilaç olup başka ilaçlar gibi interstisyel akciğer hastalığına sebep olabilmektedir. Ülseratif Kolit (ÜK) nedeni ile mesalamin tedavisi almakta olan 39 yaşında kadın hasta, öksürük, halsizlik, nefes darlığı yakınmaları ile başvurdu. Akciğer grafisi ve toraks bilgisayarlı tomografisinde bilateral yamalı konsolidasyonlar görüldü. Klinik ve radyolojik bulguların, ülseratif kolitin akciğer tutulumuna bağlı olabileceği veya mesalamine bağlı akciğer toksisitesi olabileceği düşünüldü ve mesalamin tedavisi kesildi. İzleminde, 10 gün sonraki akciğer grafisinin başvuru sırasındakine göre belirgin düzeldiği görüldü. Hastanın solunumsal şikâyetleri de geriledi. Sonuç olarak; inflamatuvar barsak hastalığının akciğer tutulumu yerine mesalamine bağlı akciğer toksisitesi düşünüldü. |
| 4. | Multipl Pulmoner Nodül Etiyolojisi: Mitral Stenoz Etiology of Multiple Pulmonary Nodules: Mitral Stenosis Funda Aksu, Alper Yurdasiper, Serdar Akyüzdoi: 10.5505/respircase.2013.08208 Sayfalar 6 - 9 Sekiz yıl önce mitral kapak replasman operasyonu geçirmiş olan 36 yaşında erkek hasta göğüs ağrısı ile başvurdu. Fizik muayenesinde göğüs ön duvarda sternotomi skarı bölgesinde şişlik, kızarıklık ve hassasiyet dışında patoloji saptanmadı. Akciğer grafisinde bilateral nodüler dansiteler mevcuttu. Bilgisayarlı toraks tomografisinde mitral kapak düzeyinde kalsifikasyon ve her iki akciğerde dağınık yerleşimli, bazıları kalsifiye çok sayıda milimetrik nodüller saptandı. İleri tetkiklerde multipl pul-moner nodül etiyolojisini açıklayacak enfeksiyöz, granulomatöz ya da neoplastik bir patoloji sap-tanmadı ve nodüller öncelikle mitral stenoza sekonder düşünüldü. Göğüs ağrısının nedeni sternal tel batması olarak saptandı ve operasyonla tel eksize edildi. İlk başvurusundan 16 ay sonra hasta hemoptizi ve şiddetli göğüs ağrısı nedeni tekrar başvurdu. Kardiyak değerlendirme ile hemoptizi ve pulmoner nodüllerin mitral kapak replasmanı operasyonu sonrası inefektif warfarin kullanımına bağlı sol atriyum basıncında yükselmelerle seyreden pulmoner konjesyona bağlandı. Romatizmal kalp hastalıkları ülkemizde halen sık olarak görülmekte olup multipl pulmoner nodül etiyolojilerinde ayırıcı tanıda düşünülmelidir. |
| 5. | Arı Sokmasını Takiben Gelişen Anafilaksi ve Diffüz Alveoler Hemoraji Anaphylaxis and Diffuse Alveolar Hemorrhage Following Bee Sting Işıl Fatma Uzel, Metin Arslan, Özkan Demirhandoi: 10.5505/respircase.2013.00710 Sayfalar 10 - 13 Böcek sokmaları ve izleyen reaksiyonlar sık görülmekle beraber, hayatı tehdit eden sistemik reaksiyonlara nadiren yol açarlar. Diffüz alveoler hemoraji (DAH), pek çok sistemik hastalığın seyrinde ve nadir durumlarda ortaya çıkabilmektedir. Klinik olarak hemoptizi, anemi, akciğer grafisinde diffüz infiltrasyonlar ve hipoksemik solunum yetmezliği tablosu görülür. Radyolojik görünüm akciğer ödemi, ciddi infeksiyon veya üremi ile benzerlik taşır. Arı sokmasını izleyen yarım saat içinde anafilaktik şok ve diffüz alveoler hemoraji tablosu gözlenen 23 yaşındaki hastayı sunuyoruz. |
| 6. | Enfekte Kistik Bronşektaziye Sekonder Gelişen BOOP (Bronşiolitis Obliterans Organize Pnömoni) ve Renal Amiloidoz BOOP (Bronchiolitis Obliterans Organizing Pneumonia) and Renal Amyloidosis Secon-dary to Infected Cystic Bronchiectasis Dilay Çimen, Mehmet Ekici, Emel Bulcun, Aydanur Ekicidoi: 10.5505/respircase.2013.19480 Sayfalar 14 - 19 Amiloidoz, amiloid olarak adlandırılan özel bir proteinin vücuttaki değişik dokularda anormal biçimde depolanması sonucunda ortaya çıkan bir grup hastalıktır. Organize pnömoni, akciğer hastalıkları içinde ender görülen ama oldukça karakteristik kliniko-patolojik özellikleri olan bir tablodur. Olgumuz nefes darlığı, öksürük, balgam, yan ağrısı yakınması ile hastanemize başvurdu. Postero-anterior akciğer grafisinde sol parakardiak sınırda heterojenite, sol sinüs kapalı olarak izlendi. Yüksek çözünürlüklü bilgi-sayarlı tomografide sol akciğer üst lob apikoposterior segmentte ve sol akciğer alt lobda yaygın buzlu cam dansitesi zemininde retikülonodüler değişiklikler, yer yer konsolide alanlar, bronşektazik değişiklikler ve hacim kaybı saptandı. Olgunun proteinürisi olması üzerine renal amiloidoz açısından böbrek biyopsisi yapıldı. Patoloji sonucu renal amiloidozis ile uyumlu geldi. Fiberoptik bronkoskopide sol alt lob mukozasında beyaz plak alanından biyopsi yapıldı. Biopsi örneği organize pnömoni (interstisyel pnömoni ve interstisyel fibrozis) bulguları ile uyumlu geldi. Bu yazıda, kistik bronşektaziye bağlı gelişen renal tutulumu olan sekonder amiloidoz ve bronşiolitis obliterans organize pnömoni olgusu sunulmuştur. |
| 7. | Kistik Fibrozisin Nadir Bir Komplikasyonu: Korneal Opasite Corneal Opacity: A Rare Manifestation of Cystic Fibrosis Sevgi Pekcan, Deniz Doğru Ersöz, Mehmet Köse, Güzin Cinel, Murat İrkeç, Ebru Yalçın, Uğur Özçelik, Nural Kiperdoi: 10.5505/respircase.2013.19483 Sayfalar 20 - 22 Kistik fibrozisli hastaların takibinde A vitamini eksikliğine bağlı göz bulguları görülebilmektedir. Korneal opasite ve gelişme geriliği ile başvurarak kistik fibrosis tanısı alan 11 aylık bir çocuğu sunuyoruz. Korneal opasite bulgusu ile tanı alan literatürde bildirilen ilk kistik fibrosis vakasıdır ve erken yaşta bu hastalarda göz bulguları nadirdir. |
| 8. | Ölümcül Bir Diş Apsesi: Desendan Nekrotizan Mediastinit Fatal Dental Abscess: Descending Necrotising Mediastinitis Atalay Şahin, Fatih Meteroglu, İsmet Rezani Toptanci, Tahir Şevval Eren, Canan Erendoi: 10.5505/respircase.2013.58066 Sayfalar 23 - 26 Mediastinit, mediastendeki hayati organların etrafında nadir görülen enfeksiyöz bir hastalıktır. Desendan nekrotizan mediastinite odontojenik, farengeal, servikal enfeksiyonlar, sternotomi veya tanı ve tedavi amaçlı girişimler sebeb olur. Zamanında tanı konulmaz ve uygun olarak tedavi edilmezse sonuç fatal olur. Tedavideki gecikme enfeksiyonun mediastene yayılmasına yol açar. Diş apsesinden muzdarip 17 yaşındaki kızda gelişen desendan nekrotizan mediastinit olgusunu sunuyoruz. |
| 9. | Akciğerde Solid Kitle Görünümü Veren Tüberküloz Olgusu Tuberculosis Case Presented with a Solid Mass Lesion in the Lung Sinem Nedime Sökücü, Levent Dalar, Cengiz Özdemir, Songül Büyükkale, Ayşegül Akbaş, Sedat Altındoi: 10.5505/respircase.2013.66376 Sayfalar 27 - 31 Tüberküloz farklı radyolojik görünümlerle ortaya çıkabilen bir hastalıktır. Sık olmamakla birlikte kitle görünümünde akciğer tüberkülozu olguları literatürde mevcuttur. Kitle görünümü ile başvuran hastalarda tüberküloz tanısından emin olmak ve eşlik eden tümör tanısını kesin dışlamak bazen zor olmaktadır. Bu yazıda, kliniğimize akciğer grafisinde kitle görünümü ile başvuran, ailesinde akciğer kanseri öyküsü olan ve sigara içen (25 paket/yıl) 45 yaşında erkek hastada tanı ve takipte yaşanan güçlükler tartışıldı. Ülkemiz gibi her iki klinik durumun da sık görüldüğü toplumlarda ayırıcı tanının içerdiği güçlükler vurgulanmak istendi. |
| 10. | Superior Sulkus Tümörünü Taklit Eden Kist Hidatik Olgusu: İntratorasik, Ekstrapul-moner, İntraossöz Yerleşim A Case of Hydatid Cyst Mimicking Superior Sulcus Tumor: Intrathoracic, Extrapulmonary, Intraosseous Location Fatih Meteroglu, Atalay Sahin, Sevval Erendoi: 10.5505/respircase.2013.68077 Sayfalar 32 - 34 Karaciğer ve akciğer dışında kist hidatik yerleşimi seyrektir. Kaburgaların kemik kısmı gibi nadir yerle-şimler, alışık olmayan semptomlara yol açabilir. Cerrahi öncesi doğru tanı önemli olup bazı vakalarda şaşırtıcı olabilir. Omuz ağrısı çeken genç bir erişkin hastada görülen birinci kosta ekinokokoz olgusu sunuldu. Akciğer grafisinde ve toraks bilgisayarlı tomografisinde superior sulkus tümörü şüphesi vardı. Lezyon rezeke edildi ve histopatolojik inceleme sonucu kist hidatik tanısı kondu. |
| 11. | Primer Pulmoner Leiomiyosarkom Primary Pulmonary Leiomyosarcoma Nurdan Şimşek Veske, Gülşah Günlüoğlu, Adalet Demir, Pelin Karadağ, Ekrem Cengiz Seyhan, Nur Ürer, Sedat Altındoi: 10.5505/respircase.2013.35744 Sayfalar 35 - 38 Leiomiyosarkom, sıklıkla uterus, retroperitoneum ve intraabdominal bölgeden kaynaklanan, düz has hücrelerinin tümörüdür. Trakeabronşiyal ağaçta düz kas hücrelerinin çokluğuna rağmen primer pulmoner kas tümörleri çok nadirdir. Kırk sekiz yaşında herhangi bir şikayeti olmayan erkek hasta, tesadüfen çekilen akciğer grafisinde lezyon saptanması nedeniyle merkezimize yönlendirilmişti. Bilgisayarlı Toraks tomografisinde sağ akciğer alt lobda 4x3 cm çaplı kitlesel lezyon izlendi. Fluorodeoksiglukoz (FDG) işaretli Bilgisayarlı Tomografi Entegrasyonlu Positron Emisyon Tomografi (PET/CT) taramada lezyonun düşük FDG tutulumu mevcuttu. Tanısal amaçlı tomografi rehberliğinde iğne aspirasyonları yapıldı. Histopatolojik tanıya ulaşılamayınca tanı ve tedavi amacıyla cerrahi planlandı. Video yardımlı toraks cerrahisi (VATS) ile alt lob wedge rezeksiyonu uygulanan hastanın postoperatif patoloji sonucu akciğerin primer leiomiyosarkomu olarak yorumlandı. |
| 12. | Bronşektazili Bir Hastada Gecikmiş Tanı: Swyer-James-MacLeod Sendromu Delayed Diagnosis in a Patient with Bronchiectasis: Swyer-James-MacLeod Syndrome Dilay Ahat Çimen, Aydanur Ekici, Emel Bulcun, Mehmet Ekicidoi: 10.5505/respircase.2013.14622 Sayfalar 39 - 43 Swyer-James/Mac Leod Sendromu (SJMS) pulmoner arter hipoplazisine bağlı unilateral hiperlüsent akciğer görünümü ve bronşektazi ile karakterize nadir görülen bir hastalıktır. Çocukluk çağında geçirilen viral bronşiolit ve pnömoniler sonrası akkiz olarak geliştiği düşünülmektedir. Kırk sekiz yaşında kadın hasta, nefes darlığı, öksürük, balgam çıkarma yakınmalarıyla başvurdu. Öyküsünden bu şikayetlerinin çocukluk yaşlarından beri tekrarladığı, 10 yıl öncesine kadar kronik bronşit, son 10 yıldır da bronşektazi ve küçük hava yolu hastalığı tanılarıyla takip ve tedavi edildiği öğrenildi. Fizik muayenesinde; solunum seslerinin şiddeti sağ alt bölgede sola göre azalmış, bilateral orta ve alt bölgede ve anteriorda kaba ralleri mevcuttu. Akciğer grafisinde; sol akciğerde hacim kaybı, radyolusensi artışı ve alt zonda bronşektazik alanlar izlendi. Bilgisayarlı tomografide; sol pulmoner arter ve dallarının kalibrasyonu sağa kıyasla belirgin azalmıştı. SJMS çocukluk ve genç erişkin dönemde teşhis edilen bir hastalık olmasına karşın, olgumuzda 48 yaşına kadar solunum şikayetleri tanımlaması nedeniyle birçok kez tetkikler yapılmasına rağmen tanı konulmamıştır. Tek taraflı hiperlüsent akciğer görünümü saptandığında bu sendromun ayırıcı tanıda düşünülmesi gerektiğini vurgulamak için sunuyoruz. |
| 13. | Sağ Pulmoner Arter Agenezisinin Eşlik Ettiği Scimitar (Pala) Sendromu Scimitar Syndrome Associated with Agenesis of Right Pulmonary Artery Dilaver Taş, Oğuzhan Okutan, Tuncer Özkısa, Ömer Ayten, Ersin Demirer, Turgut Öztutgandoi: 10.5505/respircase.2013.96268 Sayfalar 44 - 47 Scimitar sendromu, nadir bir hastalıktır ve hipogenetik akciğer sendromu olarak da bilinir. Sendrom sağ pulmoner venin, vena kava inferiora drenajı ile karakterizedir. Burada sağ pulmoner arter agenezisinin eşlik ettiği Scimitar sendromu sunuldu. Yirmi bir yaşında erkek hasta nefes darlığı, öksürük, balgam çıkarma şikayetleri ile başvurdu. Akciğer grafisinde sağ akciğerde volüm kaybı, kalp ve mediastende sağa doğru yer değiştirme izlendi. Bronkoskopik incelemede ve toraks BTde orta lob bronşu izlenmedi. Toraks BT anjiografi görüntülerinde sağ akciğer alt loba ait venin sağ hepatik vene drene olduğu ve sağ pulmoner arter çapında azalma izlendi. Akciğer perfüzyon sintigrafisinde sağ akciğerde total perfüzyon kaybı izlendi. Scimitar sendromlu hastalarda akciğer grafisinde scimitar (pala) işaretinin olması karakteristiktir. Ancak bu işaret her zaman görülmeyebilir. Akciğer grafisinde volüm kaybı ve mediastinal şifti olan genç hastalarda diğer hastalıkların yanında Scimitar Sendromu da akla gelmelidir. |